
Rabies is still a threat—but experts say it doesn’t have to be that way
Though we know how to prevent it, the virus kills about 60,000 people a year. Here’s what you need to know.
Rabies surprised public health officials earlier this year when a wild red fox bit nine people—including a United States congressman—in Washington, D.C. Within a day, a D.C. public health lab confirmed that the fox, which had been euthanized, had tested positive for the deadly disease.
Rabies kills about 60,000 people every year worldwide, particularly in rural parts of Africa and Asia. Primarily spread through animal bites, the disease is virtually 100 percent fatal once symptoms set in.
“We tend to think of it as this disease from the past, but someone dies of it every 10 minutes around the world,” says Katie Hampson, professor of biodiversity, animal health, and comparative medicine at the University of Glasgow, who specializes in the ecology of rabies. “It’s such a horrific way to die.”
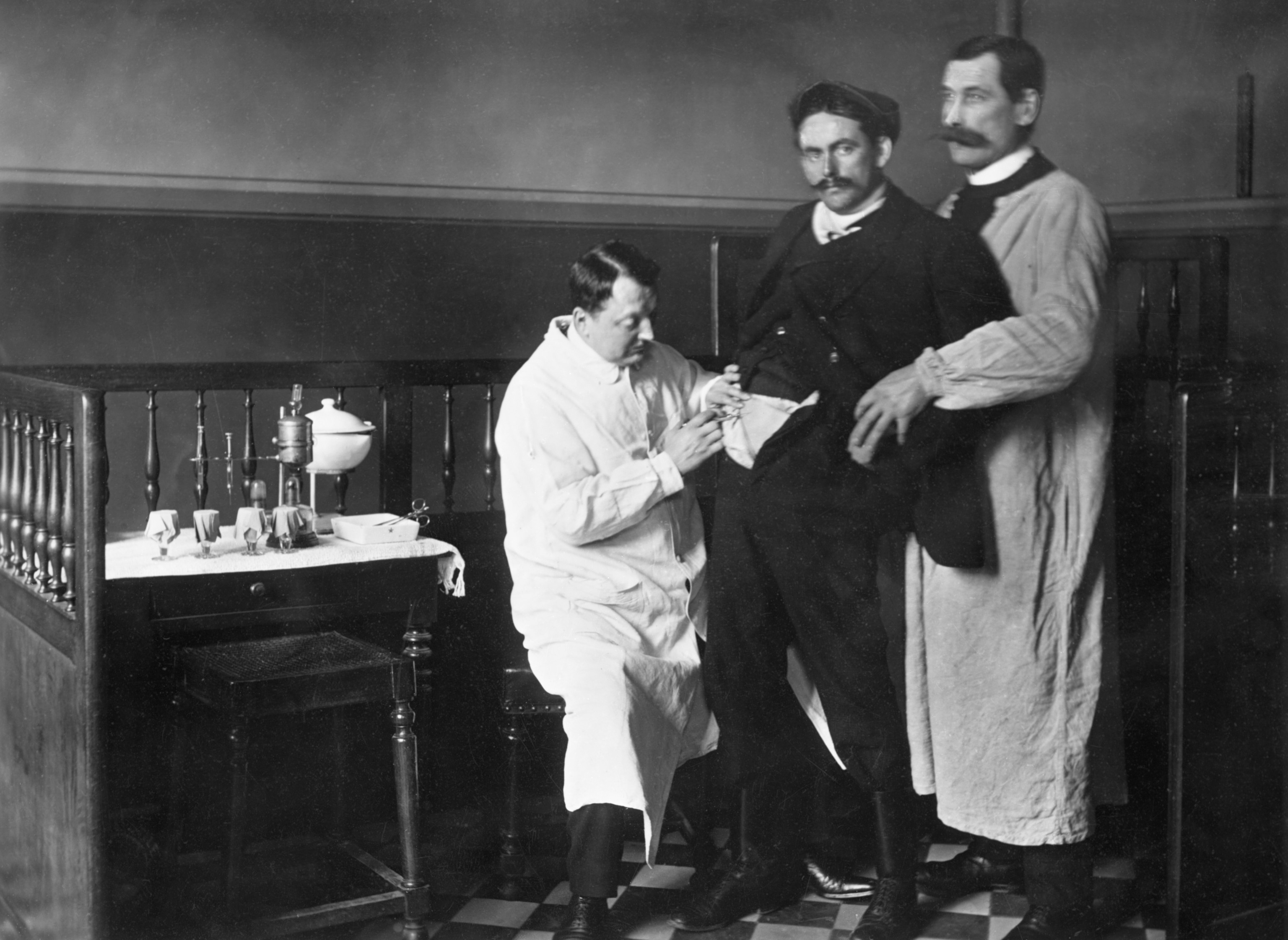
Those deaths are almost completely preventable thanks to the rabies vaccine, which was first developed by Louis Pasteur in 1885 and has been improved over time with advances in technology. As a result, the U.S. logs thousands of rabies cases among wildlife each year but only one or two human deaths.
Given all that is known about the disease, experts say that eradication would be an easy win for public health—and momentum has been building in recent years. In 2018, the World Health Organization and its partners announced a plan to eliminate human deaths from rabies by 2030. (Inside the U.S. effort to eradicate rabies in raccoons.)
("Zombie Virus" Possible via Rabies-Flu Hybrid?)
“It’s one of those issues that we really can do something about,” says Andy Gibson, director of strategic research at Mission Rabies, a United Kingdom-based charity. “There is a ray of light in it.”
What is rabies—and how is it transmitted?
Rabies lyssavirus is an RNA virus that specializes in attacking the body’s central nervous system. It’s transmitted through contact with the saliva or nervous system tissue of an infected animal. That typically takes place by animal bite or, less often, from scratches or exposure to the saliva of an infected animal.
Once it infects, the virus attaches to nerve cells and spreads along neural pathways until it reaches the spinal cord and the brain. In the brain, it begins to replicate and pass into the salivary glands—which is when clinical symptoms begin to appear.

All mammals are susceptible to rabies, but Hampson says carnivores are particularly good at transmitting it because their strong bites can easily break the skin. Dogs are most commonly associated with rabies because they live alongside humans and roam freely in many parts of the world—raising the likelihood that they’ll spread it. (Morocco has 3 million stray dogs. Meet the people trying to help them.)
But in countries where dogs are widely vaccinated against rabies, the disease remains endemic among other carnivores like foxes, raccoons, and bats. The U.S., for example, recently saw an uptick of human rabies cases linked to bats. The nocturnal animals are the country’s leading cause of rabies exposure, which the U.S. Centers for Disease Control and Prevention says is possibly because people aren’t aware of the risks that bats pose.
What are the symptoms of rabies?
When most people think of rabies, they imagine an animal foaming at the mouth and acting aggressively. But experts warn that rabies symptoms are not so straightforward and can vary widely to include seizures, anxiety, delirium, insomnia, difficulty breathing, self-mutilation, and other abnormal behavior.
“Rabies is the master of deception. It can look like anything,” Gibson says. “The only common sign is sudden death.”
According to the CDC, the earliest symptoms of rabies are similar to the flu, including weakness, fever, a headache, and tingling at the site of the bite. As the virus spreads to the brain—a journey that can take weeks or even months—a variety of more severe symptoms can emerge.
The World Health Organization describes two main manifestations of the disease: furious rabies and paralytic rabies. People or animals with furious rabies may appear agitated, become aggressive, and drool excessively, while other symptoms include hyperactivity, fear of water, and even fear of fresh air. The symptoms of paralytic rabies, on the other hand, are more understated—typically causing gradual paralysis as a patient remains calm and lucid.
What do you do if you suspect a rabies infection?
Rabies is almost always fatal once clinical symptoms set in, so it’s critical to act immediately if you or your pet has been bitten by an animal suspected to have rabies. Since bat bites aren’t always visible, experts advise reaching out to authorities if you come into contact with a bat.
But Gibson says the first step for treating rabies is something you can do on your own. “You can vastly reduce your risk of contracting rabies if you wash the wound with soap and water for 15 minutes,” he says, explaining that the rabies virus is fairly fragile and can be disrupted by soap.

Next, however, experts advise seeking care from a medical provider who can assess your risk and administer post-exposure prophylaxis (PEP)—a treatment that is 100 percent effective if administered quickly and correctly. PEP typically includes four shots of the rabies vaccine taken over two weeks, as well as a dose of rabies immune globulin, a serum that neutralizes the virus at the site of the bite and offers protection as the body mounts an immune response.
The rabies vaccine is unique in that it is typically administered after an infection rather than as a preventive measure. Hampson says that’s because most people—particularly in countries that have controlled rabies in dogs—are unlikely to be exposed. However, those who are at risk due to their jobs or who travel to a high-risk country may consider a pre-exposure vaccination.
“You’d be very unlucky to be bitten by a rabid dog, but thousands of people who live in these countries get bitten every day, so it’s a non-negligible risk,” Hampson says.
What threat does rabies pose to humans?
For people who live in wealthy countries, the risk of getting rabies in the first place is extremely low. That’s because scientists know what works to prevent rabies: generating herd immunity by vaccinating at least 80 percent of the local host population, typically domestic dogs.
“If you can achieve that critical herd immunity, you stop transmission—you stop the cycle,” says Louis Nel, executive director of the Global Alliance for Rabies Control, an NGO that works with governments and international organizations to fight rabies. “That’s how you eradicate the virus.”
In the U.S., the number of human rabies deaths fell from more than a hundred a year in the early 20th century to just one or two a year since 1960, when the country began to vaccinate dogs. There have been similar successes in western Europe and, most recently, in Latin America and the Caribbean, where cases have declined 95 percent since 1983 to make the region nearly rabies-free.
That’s not to say there’s zero threat in these countries. In addition to the risk posed by other wildlife such as foxes and raccoons, rabid dogs can cross borders and reintroduce the disease. Even in the U.S. there are occasional reports of rabies among imported dogs, and roughly a quarter of human rabies cases involve people who are infected while traveling.
But the threat is vastly higher in countries that have not controlled rabies in dogs. In 2018, a WHO Rabies Modelling Consortium study published in the Lancet estimated that more than a million people would die of rabies between 2020 and 2035 if those countries don’t take action.
What can be done to control rabies globally?
The WHO and its global partners have called for the elimination of human rabies deaths by 2030. Given that we already know how to prevent rabies, experts say what’s really needed in affected countries is the political will and improved health care infrastructure.
“It’s not always logical for governments to realize that this is an area where they could make a big difference to public health,” Nel says. “So that’s why we need to build the case for investment.”
In 2013, Mission Rabies was able to do just that when it began working in Goa, India. At the time, the state government was finding only about five rabid dogs a year. But increased surveillance efforts showed a much more serious problem with two positive cases a week. “We suddenly found there was rabies everywhere,” Gibson says.
Armed with a better understanding of the problem, Goa signed onto a years-long program to eliminate rabies by vaccinating more than 95,000 dogs every year to reach 70 percent vaccination coverage. Aided by smartphone technology making it easier to find the dogs and track progress, Goa has now eliminated human rabies. (Why adopting street dogs is gaining popularity in India.)
The 2018 WHO modelling study also recommended providing low-income countries with better access to post-exposure treatment—which Hampson, the lead author of the paper, says is a cost-effective way to keep people safe while countries work to reach herd immunity in dogs. The Global Alliance Vaccine Initiative has since added the rabies vaccine to its portfolio.
However, COVID-19 has complicated these global efforts, diverting resources away from rabies to tackle an even graver threat. Nel admits the Zero by 30 target may be slipping away—but adds that it’s an important goal to aim for. Gibson agrees, adding that even small progress against rabies will still help save many lives.
“The allure of eradication is very appealing,” he says. “But there’s a lot of good we can do just by taking the steps we can in the meantime.”