Can vitamin D lower risk of heart attack? Here’s what the science shows.
Low levels of vitamin D seem to raise your risk of heart attack but scientists are still figuring out why—and whether supplements might help protect you.

Vitamin D has long been known to play an important role in the body—and not getting enough of it has been linked to a number of health issues, including an increased risk of certain types of cancers and autoimmune diseases. But there’s one link that scientists are still researching.
“There is a long association with vitamin D and heart health,” says B. Keith Ellis, a cardiologist at Houston Methodist Hospital in Texas, pointing to a raft of studies linking low vitamin D to cardiovascular risk.
But scientists are still trying to figure out why not getting enough vitamin D seems to be bad for your heart. And it’s even less clear whether taking vitamin D supplements could help—until now.
Scientists presented the results of a recent study, called TARGET-D, at the American Heart Association’s annual meeting in New Orleans, Louisiana, showing that patients who took vitamin D supplements designed to reach a blood level between 40 and 80 ng/mL, thought to be healthiest for the heart, were 50 percent less likely to have a heart attack.
“The effects are promising,” says Markus Herrmann, a researcher at the Medical University of Graz in Austria, who was not involved in the study. As Herrmann notes, this is the first study to have a specific target for vitamin D levels.
(You probably aren't getting enough vitamin D—here's what the experts say.)
In previous studies, there was a lot of variation in how much vitamin D patients already had naturally at the beginning of the study, as well as how much supplementation they received. This has made it hard to tease out the specific effects of vitamin D on heart health, as well as which patients might benefit the most.
“This study is very important in that regard,” Ellis says, “showing that people who have had a heart attack, if you can keep their vitamin D levels between 40 and 80 ng/mL, you can reduce the risk of a second heart attack.”
But it’s far from the last question they hope to answer about the role vitamin D plays in protecting your heart.
Vitamin D is essential—and yet most people can’t get enough
Vitamin D does a lot for your body. It plays a role in bone metabolism, along with calcium. It also plays a role in immune health and the functioning of brain and muscle cells.
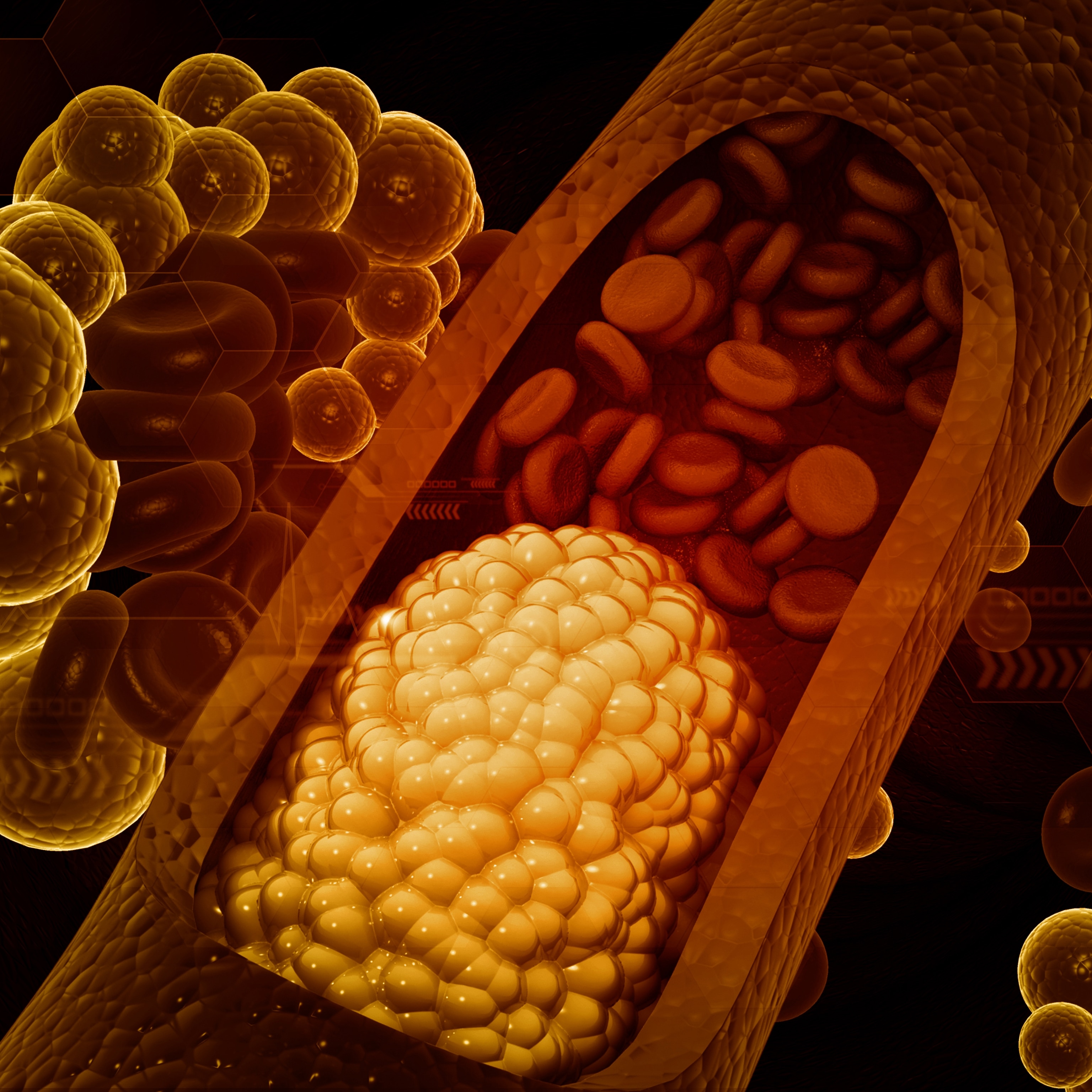
Vitamin D’s role in heart health is thought to be linked to its anti-inflammatory properties, with heart disease driven, in part, by inflammation. Vitamin D also plays a role in lowering blood pressure and regulating blood sugar levels, both of which can contribute to the risk of a heart attack.
However, it’s also possible that low levels of vitamin D are what is known as a confounding factor, where the actual cause of heart disease is due to a related factor. In the case of vitamin D, since it is produced by the body after exposure to sunlight, vitamin D levels might simply be a byproduct of how active a person is.
“Vitamin D levels go up with physical activity outdoors, and so people who are physically active outdoors are also going to have lower risks of heart disease,” says Rachel Neale, a researcher at QIMR Berghofer Medical Research Institute in Herston, Australia. So when observational studies show that people with high levels of vitamin D are healthier, she says, it might not be because of the vitamin D itself but because of their activity levels.
(The truth about immune-boosting supplements.)
But it’s often hard to get enough vitamin D. The nutrient is found in certain foods such as fish such as salmon or sardines, yet because these foods aren’t a significant part of most diets it has also been added to foods such as milk or cereals as a form of supplementation. Vitamin D can also be produced by the body after exposure to direct sunlight.
Worldwide, an estimated one billion people are deficient in vitamin D, with levels varying depending on a person’s diet, how much sun exposure they receive, and whether they have any additional health conditions, such as chronic kidney disease, that might predispose them to a deficiency. Blood levels of vitamin D can also vary throughout the year, with people in northern climates often experiencing lower levels in the winter.
This is why scientists have been keen to discover whether taking supplements—such as pills or gummies—could help make a difference.
What earlier research showed about vitamin D supplements
Before now, there have been two major trials looking at the effects of vitamin D supplementation on parameters of heart health: the D-Health Trial and the VITAL Trial, as well as a number of smaller trials. Neither trial showed any significant benefits of taking extra vitamin D, although the D-Health trial did find borderline significant effects for reducing the risk of a heart attack.
(Why heart attacks are rising in young adults—and what to watch out for.)
But researchers point out that the study designs weren’t capable of answering the overall question of what effect vitamin D supplementation has on heart health. Rather, they were observing the effects of a certain group of people taking vitamin D for a limited amount of time.
“Both [trials] recruited people who were not predominantly vitamin D deficient,” says Neale, who led the D-Health trial.
There is some question of whether vitamin D supplements are really only beneficial for people who are deficient, or if there is a benefit to increasing levels in a person who already has sufficient amounts of vitamin D.
“The trials set out to say, does giving a particular dose of vitamin D for a particular length of time, to a certain age of people, at a point in their life course, affect their heart health?” Neale says. “That’s the question we can answer.”
But that didn’t necessarily mean that there wasn’t a broader benefit to taking vitamin D supplements. It may have just meant that researchers needed to study a different group of people, switch up the dosing in some way, or give vitamin D for a longer period of time.
“Vitamin D is cheap, safe and effective, and is likely to have benefits,” Neale says, adding that “there may be some people for whom we might discover that it’s critically important.”
This is what scientists had hoped to test in the new study presented at the American Heart Association’s annual meeting.
What the latest research shows
As its name suggests, the TARGET-D study took a more targeted approach to studying vitamin D and heart health.
In the study, 630 patients were enrolled within 30 days of having a heart attack, placing them at a much higher risk for having a second heart attack.
Patients were then randomized to receive either a placebo or a dose of vitamin D specifically tailored to raise levels in their body to a target concentration of between 40 and 80 ng/mL—the level that’s considered optimal for heart health.
“They wanted to make sure they had the maximum effect and maximum benefit,” says Eleanor Levin, a cardiologist at Stanford University Medical School, who was not associated with the study. In Levin’s experience, if a patient is low in vitamin D, she has typically recommended supplementing until their levels are above 30 ng/mL, which is considered to be a normal level.
To achieve these levels, about half of the patients had to take higher-than-usual doses of vitamin D, about 5,000 IUs a day. (By comparison, the recommended daily amount of vitamin D supplementation is typically between 800 to 1,000 IUs.)
(Why vitamins A and E can cause harm in large doses.)
“The average time to get to a therapeutic threshold took about five months,” says Helen May, a researcher at the University of Utah, and one of the authors of the study.
Patients were followed for an average of four years. Since this was a high-risk population, there were a total of 107 major cardiac events reported during the course of the study, including heart failure hospitalizations, heart attacks, stroke, and death. Patients who received the vitamin D supplements experienced a 50 percent reduction in the risk of having a second heart attack, as well as an overall reduction in the risk of having a major cardiac event.
Looking ahead
TARGET-D is an important study, in that it has established that a high-risk population of patients can benefit from supplementing vitamin D to a target concentration of between 40 and 80 ng/mL. This study will need to be repeated in a larger sample of patients.
“The limitation is that it is relatively small in terms of size, but the effects are promising,” Herrmann says. “I would like to see more of these studies.”
Researchers will also want to answer the question of whether a similar vitamin D supplement regimen can help in other scenarios, such as patients who haven’t had a first heart attack.
Moving forward, it’ll also be important to make sure that patients are taking the right amount of vitamin D, as too much can be just as problematic as too little. Although low levels of vitamin D are associated with a number of health issues, including fatigue, malaise and muscle aches, too much vitamin D can result in issues such as kidney stones and excessive levels of calcium in the blood.
But as researchers sort through these remaining questions, they have one key piece of advice for anyone curious about the heart benefits of vitamin D: “If your vitamin D level is low, or you are concerned, you should consult with your physician for the appropriate dose,” says Ellis.