
Some US Hospital Infections Dropping, But Superbug Risks Are High
Fifteen years after a national report exposed how many Americans were being made sick and dying because of medical errors, some infections caused by hospitals are decreasing, according to the Centers for Disease Control and Prevention. But in a report published Thursday, the agency warns that the incidence of other infections remains stubbornly high, despite fixes that are simple in some cases—and the proportion of them that are antibiotic-resistant is, in its director’s words, “chilling.”
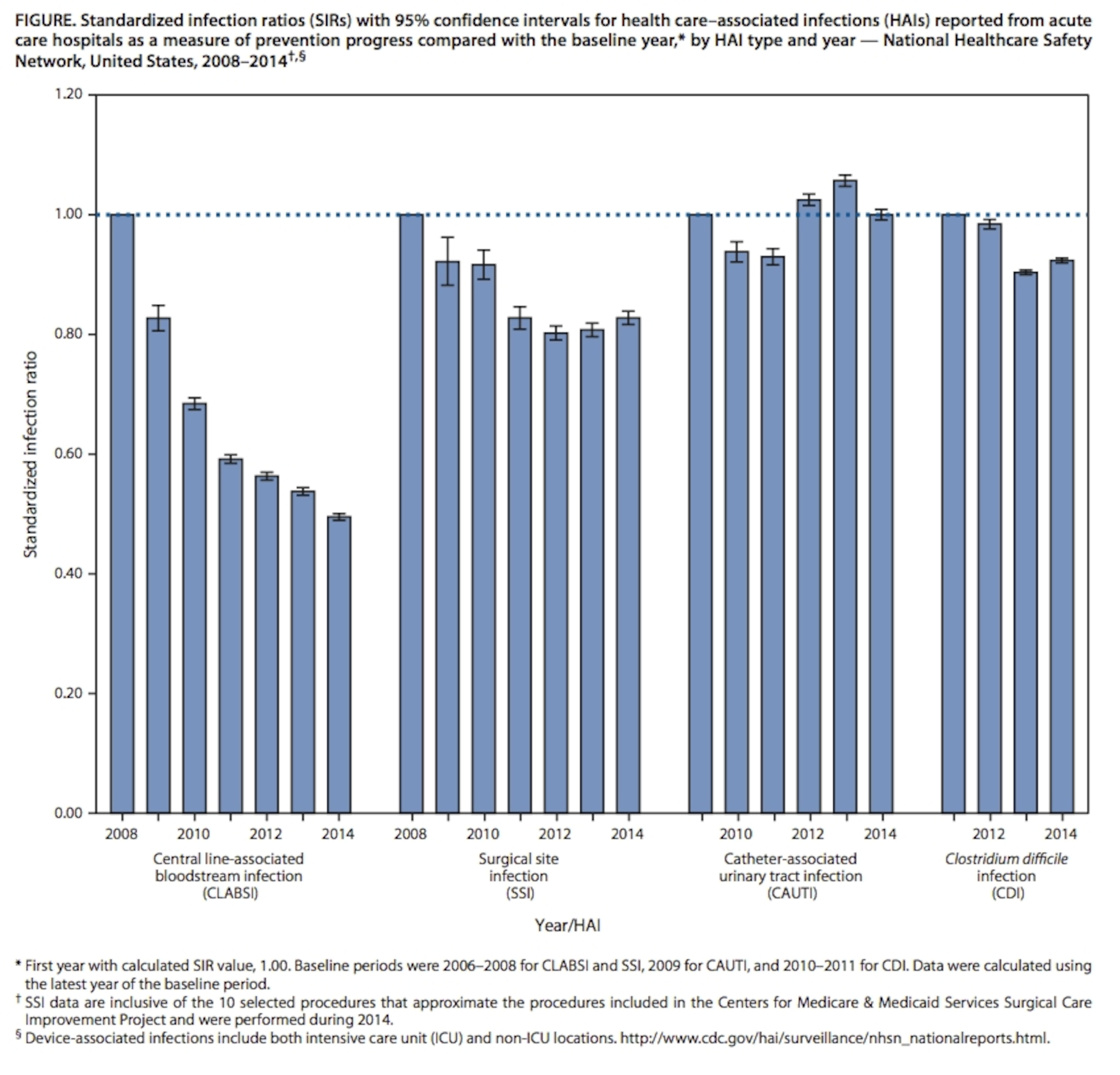
Drawing on data from its National Healthcare Safety Network, which compiles reports from 4,000 hospitals, 1,135 rehab facilities and 501 long-term acute care hospitals (which house severely ill patients who need ICU-level care for a long time), the agency reported that in 2011, 722,000 “healthcare-associated infections” occurred, and approximately 75,000 patients died. Between 2011 and 2014, it said:
- for central line-associated bloodstream infection, which start from a tube threaded near the heart to deliver medications: a 50 percent reduction in hospitals and 9 percent in long-term acute care hospitals;
- forurinary-tract infections caused by catheters inserted into the bladder: no change in hospitals, an 11 percent reduction in long-term acute care hospitals, and a 14 percent reduction in inpatient rehab facilities;
- for infections in surgical incisions, a 17 percent reduction in hospitals;
- and for Clostridium difficile infections—the devastating antibiotic-associated diarrhea that is a signal for high antibiotic use and insufficient hygiene—an 8 percent reduction in hospitals.
But while those reductions are good news, the troubling aspect of the report is the percentages of hospital-caused infections that are antibiotic-resistant. In 2014, the CDC said, 14.9 percent of those infections were resistant. Breaking those down:
- in hospitals, 18 percent of central line-associated bloodstream infections, 15 percent of surgical-site infections and 10 percent of catheter-associated urinary tract infections were resistant;
- in rehab facilities, 12 percent of urinary-tract infections were resistant;
- and in long-term acute care hospitals, 28 percent of central line-associated bloodstream infections and 29 percent of cather-associated urinary tract infections were resistant.
In a phone briefing with reporters, Dr. Thomas Frieden, the CDC’s director, called the high levels of resistance in infections in long-term care facilities—more than one in four of each infection— “chilling.” Asked how he would describe the rate in regular hospitals, which exceeds one in seven, he replied: “deeply concerning.”
According to the CDC’s data, 4 percent of patients develop an infection as a result of a hospital stay. Many of those, Frieden said, are the responsibility of healthcare personnel who fail to follow simple, known procedures, from washing hands to neglecting rules for installing catheters to continuing antibiotics beyond when they are needed. “Doctors are the key to stamping out superbugs,” he said. “No one should get sick when they are trying to get well.”
But, Frieden said, forcing down rates of healthcare infections and resistance in hospitals will also require investment in new diagnostics and patient records, beyond what hospitals can currently afford—especially since resistant bacteria can be carried into hospitals from longterm care facilities, which may have fewer staff and less resources for infection control.
Dr. Peter Pronovost, director of the Armstrong Institute for Patient Safety and Quality at Johns Hopkins—an early champion of cockpit-style checklists to prevent healthcare infections, who was also on the call to reporters—added: “We need things to better identify organisms faster, so we could implement appropriate checklists. We need to better understand when surfaces are clean very much earlier, so we know if our cleaning efforts are effective. And we need to have better regional and networked information systems, so we know what resistance patterns are in community hospitals and longterm care facilities, and be able to link them when patients come to acute-care hospitals and then go back again.”
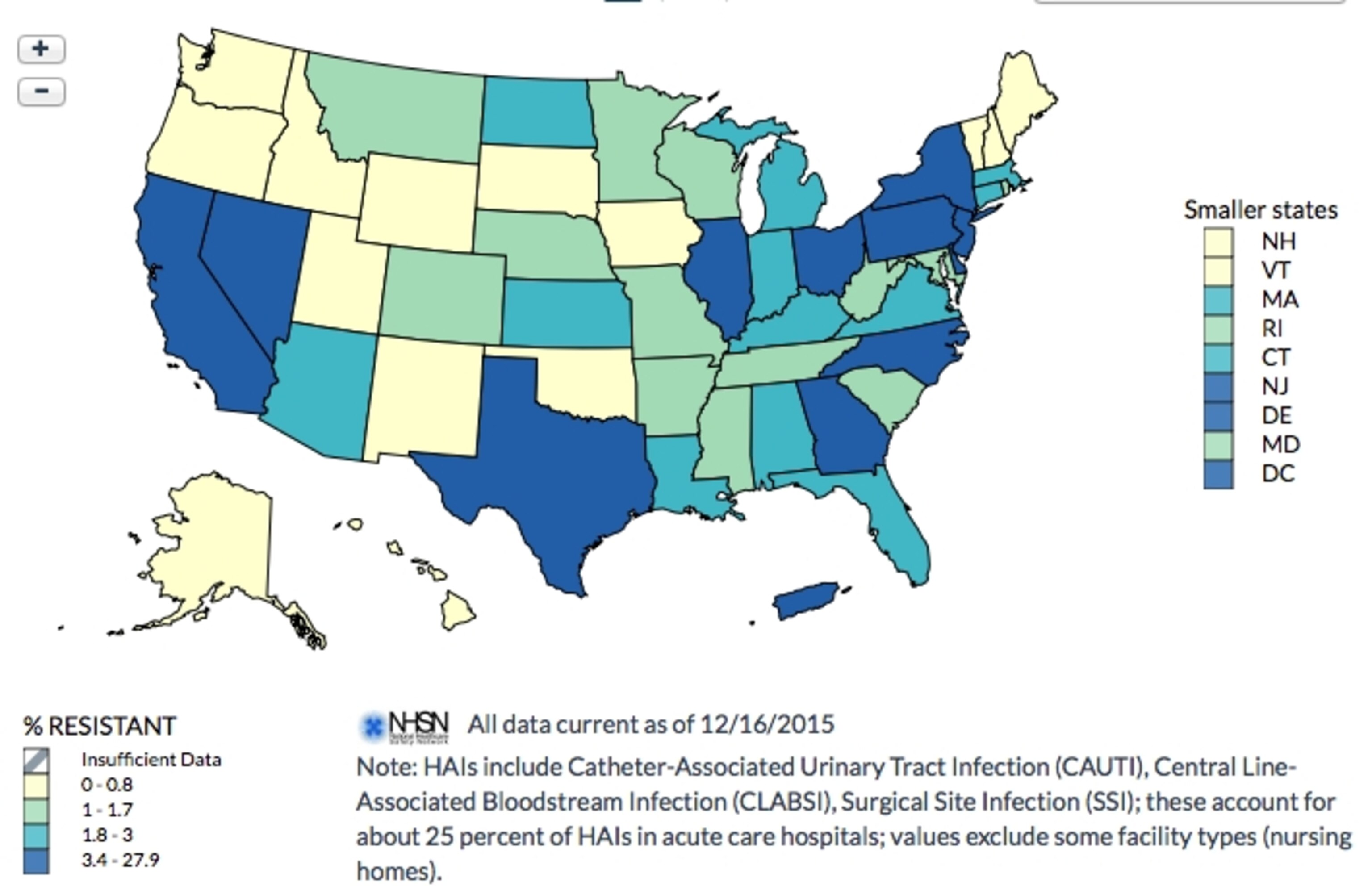
At the same time as it released its report, the CDC launched an Antibiotic Resistance Patient Safety Atlas, a web-based interactive that creates data visualizations of hotspots of resistant infections, nationally and by state, by drawing from the National Healthcare Safety Network database. Using the atlas, here is what MRSA, drug-resistant staph, looks like in hospital infections from 2011 to 2014:

And here is the occurrence of CRE—carbapenem-resistant Enterobacteriaceae—the “nightmare bacteria” that respond to only one or two antibiotic families:
The CDC’s report was released Thursday in many pieces: in addition to the atlas, a press release, a scientific paper, a simpler factsheet, and a state-by-state report assessing progress against national benchmarks.