
The world seemed to stop on April 12, 1955, when officials at the University of Michigan School of Public Health announced that Jonas Salk had developed a vaccine that protected against polio.
As the news was broadcast across the country, Paul Offit, director of the Vaccine Education Center at the Children’s Hospital of Philadelphia, remembers that businesses and schools closed so that Americans could celebrate, and churches and synagogues held special prayer services. His own mother cried at the news, relieved that her children would finally be safe from the disease that was known to paralyze its victims, leaving them unable to walk or even breathe.
“This was a major event, which tells you how scared people were of polio—and for good reason. If it paralyzed your ability to breathe, you were well aware of what was happening,” Offit says. Many patients stricken by polio were forced to rely on an iron lung for years.
In the decades since Salk’s breakthrough, wild polio has been eliminated in all but two countries, Afghanistan and Pakistan. Yet the disease has crept back in countries that believed polio was long behind them. In recent weeks, the United States has been shaken by the news that a New York man was left paralyzed by polio, the nation’s first such case in nearly a decade. Israel also reported a case of paralytic polio in February.


“You can assume that when you see that case in New York City of a man who wasn’t vaccinated, who now is infected…that he represents the tip of an iceberg,” Offit says, explaining that paralytic polio is so rare that it suggests there are many other cases that have so far gone undiagnosed. And, indeed, the virus has since been found in the wastewater of New York, Jerusalem, and London.
Offit and other experts warn that all this suggests that growing numbers of unvaccinated people have left some communities particularly vulnerable to polio’s most horrific outcomes. (Why sewage is one of the best tools for predicting COVID-19 outbreaks.)
Here’s what you need to know about the risks of polio, vaccines used to combat it, and where we stand in the global push to eradicate the virus.
What is polio—and how did we almost wipe it out?
Polio is an ancient disease caused by three strains of poliovirus. Perhaps its earliest depiction was a circa-1400 B.C. Egyptian funerary tablet that shows a priest with a withered leg walking with a cane. First clinically described in 1789, the virus primarily spreads through contact with the feces of an infected person and is infamous for causing severe paralysis.
Paralytic polio is rare, however. Most people who are infected don’t have any symptoms at all and a quarter only experience flu-like symptoms. According to the U.S. Centers for Disease Control and Prevention, only about one in 200 people—or one in 2,000, depending on the virus strain—develop paralysis.

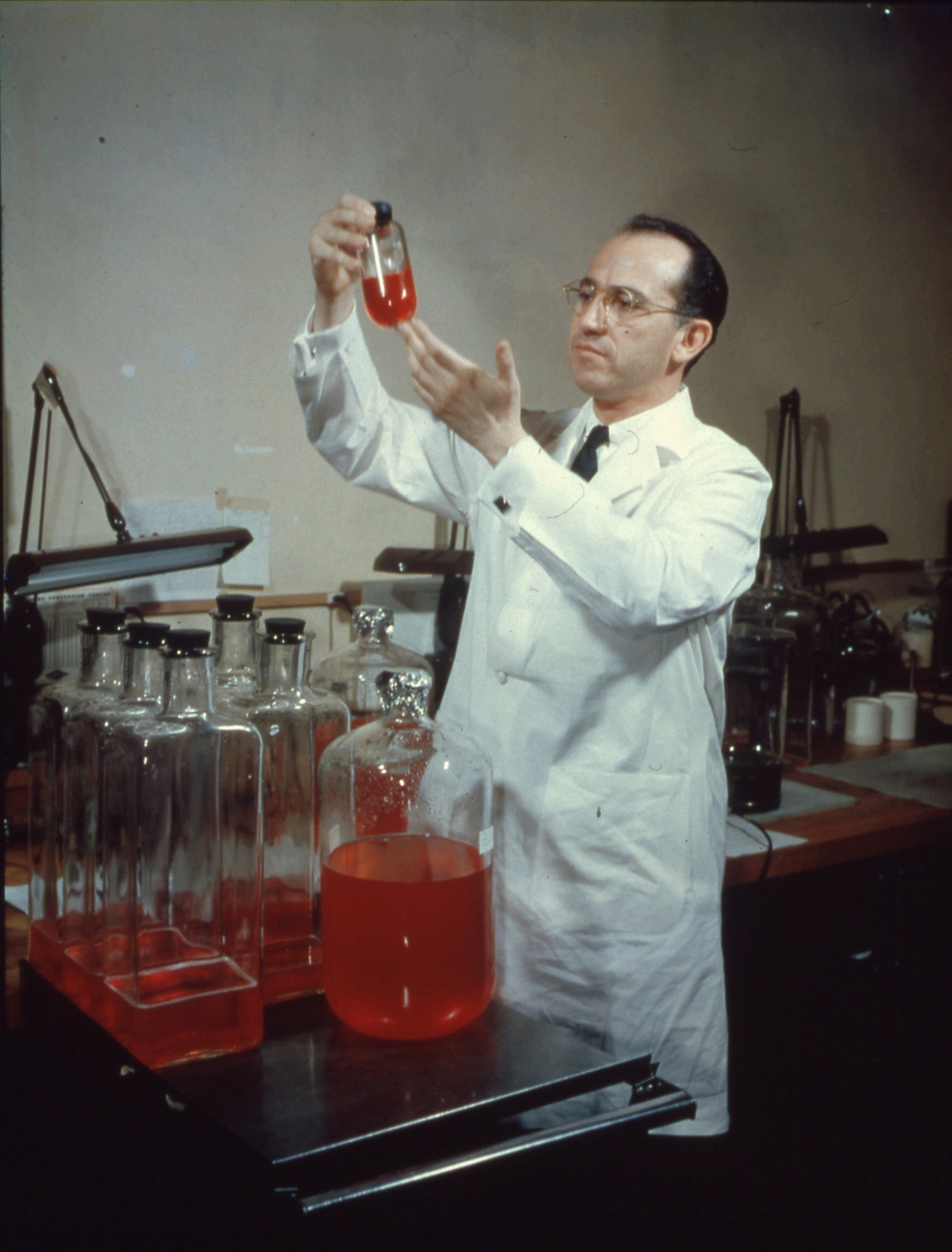
Still, polio was so rampant in the 20th century that the U.S. recorded about 16,000 cases of paralytic polio a year by the time Salk developed his vaccine. Developed using an inactive form of the poliovirus that can induce immunity without causing disease, Salk’s viral vaccine was administered in a series of injections. It quickly proved safe and effective: Case numbers dropped from 29,000 new cases in 1955, when the shot was licensed, to fewer than 6,000 within two years. (Here’s how teens made polio vaccination hip in the 1950s.)
Just as Salk’s vaccine was circulating, another American researcher, Albert Sabin, was working on a polio vaccine that used a weakened form of live virus, which at the time was thought to provide more enduring immunity. Taken orally rather than by injection, the Sabin vaccine was shown to induce an immune response in the gut, critical to stopping the transmission of wild poliovirus. What’s more, the weakened virus could spread and induce immunity when vaccinated people came in contact with those who hadn’t yet had the jab.
“The invention of the poliovirus vaccine with Salk and Sabin competing was just a major medical achievement and a real revolution in global health,” says Daniel Caplivski, an infectious disease specialist at the Icahn School of Medicine at Mount Sinai in New York.

Thanks to a mass immunization campaign—which gained momentum in the 1980s after the eradication of smallpox—polio has nearly been eliminated worldwide. In fact, two of the three strains of wild polio have been “certified eradicated,” says Ananda Bandyopadhyay, deputy director of polio technology, research, and analytics at the Bill & Melinda Gates Foundation.
Today, polio remains a routine immunization, one that’s required to enroll a child in public school in every U.S. state. Vaccine coverage is overwhelmingly high in most countries and protection from both the vaccines is now believed to last a lifetime.
So why are there still polio outbreaks?
Although mass immunization campaigns have eliminated wild polio from much of the world—most recently in Nigeria and India—there have at times been outbreaks in countries that have eliminated it. In those cases, the disease is triggered not by wild virus but by something called vaccine-derived polioviruses—mutated forms of the weakened live virus in Sabin’s oral vaccine.
These rare viruses develop in communities where immunization against polio is persistently low, giving the weakened virus in the vaccine plenty of time to find enough unvaccinated people in the community to infect. As it replicates, the viral genome can mutate and revert to a virulent form of the virus in what Bandyopadhyay describes as a “desperate attempt to survive.” Although people who are vaccinated remain protected from the new strain, anyone who is unvaccinated risks paralysis.
Researchers have known about this phenomenon for decades, Bandyopadhyay says. In the early 2000s, some countries like the U.S., which had already eliminated polio, stopped administering the oral vaccine in favor of Salk’s original inactivated vaccine, which cannot cause new infections. But for the rest of the world, that wasn’t practical.
Sabin’s oral vaccine is more affordable than the inactivated vaccine, and because it’s administered in drops rather than by injection, it is easy for volunteers to carry into remote villages and administer with minimal training. The oral vaccine is also more effective for stopping transmission of the virus, which is essential for eradication.
“I think that is probably the best way to eliminate the virus from the world—but it comes with a price,” Offit says, adding that these vaccine-derived strains of polio are likely circulating around the world, even in places where it hasn’t been detected because we’re simply not checking for it. “If we let our guard down as happened with this community in New York, then polio can come back.”
How can you protect yourself?
Scientists stress that vaccination is the key to ending all polio outbreaks. Unlike COVID-19 variants that can evade vaccine immunity, the polio vaccines are broadly protective against wild polio and the vaccine-derived polioviruses. Meanwhile, high vaccine coverage keeps communities safe by making it harder for the virus to find a new host.
Offit points to a 1972 polio outbreak at a Christian Science boarding school in Greenwich, Connecticut, that paralyzed eight children who had not been vaccinated. Although there were concerns at the time that the virus could spread into the surrounding communities, Offit says this never came to pass, thanks to the high levels of protection in those areas.
What does all this mean now? If you’ve been vaccinated already, there’s nothing more to do to protect yourself. But if you haven’t gotten a jab, now is the time. Even if you aren’t sure whether you’ve been vaccinated, Caplivski says both the polio vaccines are so safe that there’s really no downside either to getting a booster dose or taking the whole series of shots.
In New York, he adds, the Department of Health has asked medical providers to ensure kids are up to date on their vaccines—especially given evidence that the COVID-19 pandemic has disrupted routine childhood immunizations globally. In the United Kingdom, public health officials have launched a polio vaccination campaign to reach kids ages 1 through 9.
But scientists are particularly concerned about reaching the communities that have so far refused to vaccinate their children. “I think there’s a tendency when we live for many years without the memory of some of these childhood illnesses to take for granted the basic effectiveness of the vaccines,” Caplivski says, adding that often parents decide not to vaccinate their kids because they don’t understand the risks of polio and other childhood diseases like measles that have mostly been eliminated.
Offit agrees. “That’s the frustrating thing here,” he says. “There are so many things in medicine we don’t know, there’s so many things we can’t do. This we know and this we can do. To watch people reject it, it’s painful.”
What else is needed to end polio?
Containing the threat of vaccine-derived polioviruses will require a shift away from the oral vaccines that have been so essential to global eradication. But while the goal is to abandon them entirely, Bandyopadhyay says the oral vaccines are still needed to reach communities in Afghanistan and Pakistan where polio remains endemic.
That’s why researchers with the Global Polio Eradication Initiative (GPEI)—a public-private organization that includes the Gates Foundation, World Health Organization, Rotary International, and other partners—have come up with an interim solution: a version of the oral vaccine that cannot revert to an infectious state.
“What we have done is to tighten the loose ends of the existing vaccine virus,” Bandyopadhyay says. He explains that researchers have pinpointed the specific part of the weakened live virus in the oral vaccine that is prone to reverting to an infectious state. By tweaking the genetic instructions that encode the structure of the virus they have attempted to stabilize it.
“So far the data looks exceptionally promising,” Bandyopadhyay says. About 450 million doses of the novel oral polio vaccine (nOPV2) have been administered globally since the World Health Organization listed it for emergency use in November 2020. In the time since, Bandyopadhyay says there haven’t been any new outbreaks of vaccine-derived poliovirus in the areas where it was administered. Sewage surveillance shows that the virus is not mutating back to a virulent state.
Once all forms of wild virus transmission stop, Bandyopadhyay says the GPEI plans to switch to using the inactivated vaccine to eliminate the potential for vaccine-derived polioviruses to emerge. But in the meantime, he says, it doesn’t matter: “If you can reach that last child in that last community with the vaccine, irrespective of the vaccine choice, the job is done.”
Ultimately, this will rest on reaching the growing community of people who have resisted vaccines. Will a new outbreak change their minds? If not, Offit says it doesn’t bode well for the future. “If polio doesn’t scare you, what does?”