Scientists Create Personalized Stem Cells, Raising Hopes for Diabetes Cure
Insulin-producing cells could one day replace cells damaged by diabetes, a step toward curing the disease.
Regenerative medicine took a step forward on Monday with the announcement of the creation of the first disease-specific line of embryonic stem cells made with a patient's own DNA.
These cells, which used DNA from a 32-year-old woman who had developed Type-1 diabetes at the age of ten, might herald the day—still far in the future—when scientists replace dysfunctional cells with healthy cells identical to the patient's own but grown in the lab.
The work was led by Dieter Egli of the New York Stem Cell Foundation (NYSCF) and was published Monday in Nature.
"This is a really important step forward in our quest to develop healthy, patient-specific stem cells that can be used to replace cells that are diseased or dead," said Susan Solomon, chief executive officer of NYSCF, which she co-founded in 2005 partly to search for a cure for her son's diabetes.
Stem cells could one day be used to treat not only diabetes but also other diseases, such as Parkinson's and Alzheimer's.
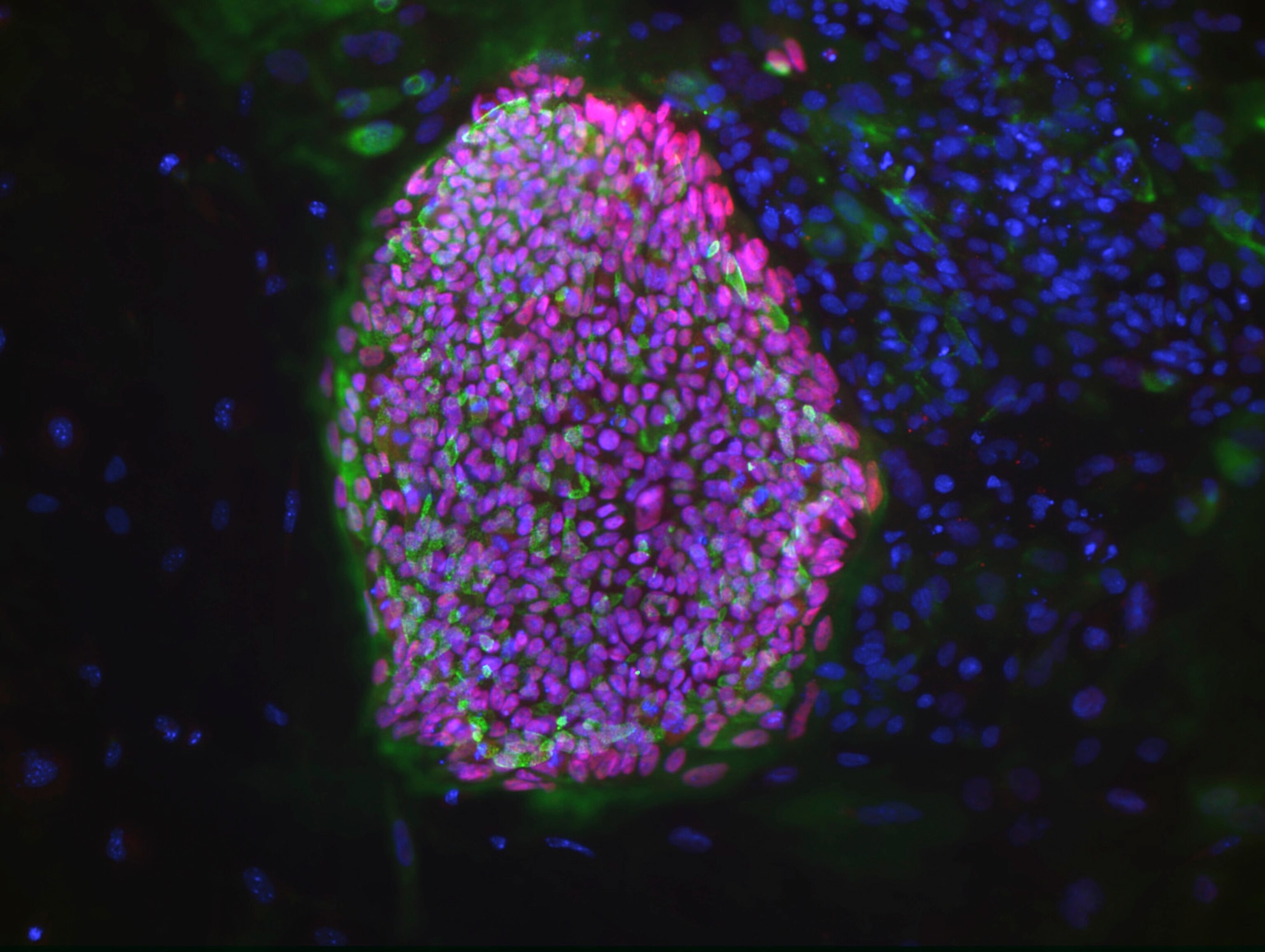
Embryonic Stem Cells Morph Into Beta Cells
In Type 1 diabetes, the body loses its ability to produce insulin when insulin-producing beta cells in the pancreas become damaged. Ideally this problem could be corrected with replacement therapy, using stem cells to create beta cells the body would recognize as its own because they contain the patient's own genome. This is the holy grail of personalized medicine.
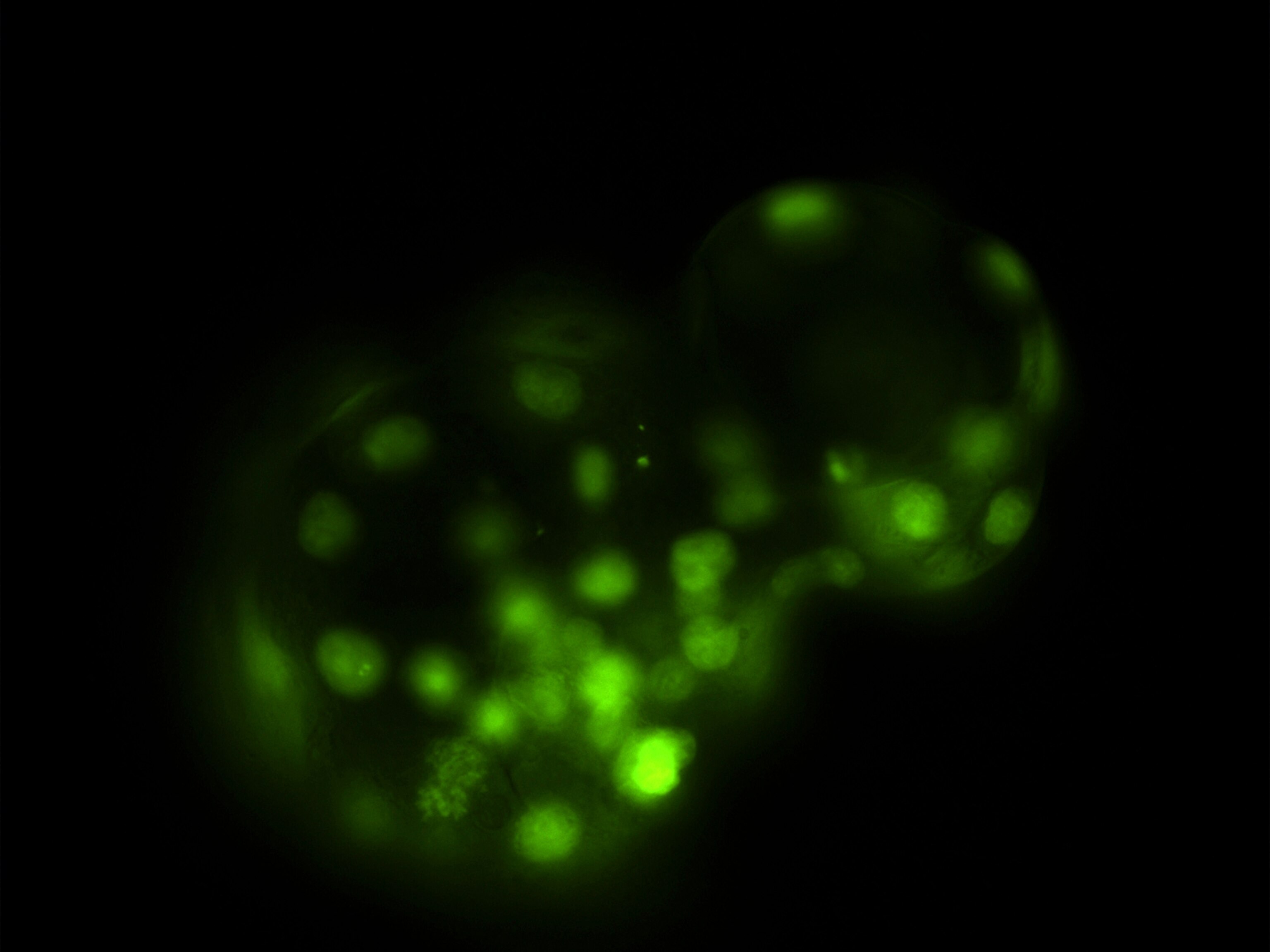
To create a patient-specific line of embryonic stem cells, Egli and his colleagues used a technique known as somatic cell nuclear transfer. They took skin cells from the female patient, removed the nucleus from one cell and then inserted it into a donor egg cell—an oocyte—from which the nucleus had been removed.
They stimulated the egg to grow until it became a blastocyst, a hundred-cell embryo in which some cells are "pluripotent," or capable of turning into any type of cell in the body. The researchers then directed a few of those embryonic stem cells to become beta cells. To their delight, the beta cells in the lab produced insulin, just as they would have in the body.
This research builds on work done last year in which scientists from the Oregon Health and Science University used the somatic cell nuclear transfer technique with skin cells from a fetus. It also advances previous work done by Egli and his colleagues in 2011, in which they created embryonic stem cell lines with an extra set of chromosomes. (The new stem cells, and the ones from Oregon, have the normal number of chromosomes.)
Shoukhrat Mitalipov, director of the Center for Embryonic Cell and Gene Therapy in Oregon, praised Egli's work: "Personally knowing Egli and his team, I have no doubts that they derived stem cells from nuclear transfer."
Cure for Diabetes Still a Long Way Off
Replacing damaged cells with new ones created through stem cell technology could "dramatically change treatment and possibly even [provide] cures" for diseases like diabetes, Solomon said.
But with diabetes, replacement therapy comes with a catch: autoimmunity. For unknown reasons, in Type-1 diabetes the immune system destroys the body's own beta cells, mistakenly treating them as invaders. If new beta cells were introduced—even ones derived from the patient's own cells—the immune system would attack them too. Scientists have yet to devise a way around this.
Another problem with the technique, according to geneticist George Church of Harvard Medical School, is "where to get the oocytes. Human oocytes are currently precious," he said, because retrieval is not simple: Donors have to go through hormonal treatment, and egg retrieval involves minor surgery. "I can imagine ways to alleviate this," he said, "but the authors don't address this."
Because it involves the creation and destruction of human blastocysts, the somatic cell nuclear transfer technique remains politically and ethically charged. Some also worry that the method might be used one day for human cloning or to create designer babies.
Most stem cell labs now use a less controversial technique discovered in 2007, which converts adult cells into stem-cell-like induced pluripotent stem (iPS) cells that can be grown into particular cell types, such as beta cells.
NYSCF is supporting research using both techniques, because each one has a function, Solomon said. The iPS technique is excellent for drug screening and disease modeling, but nuclear transfer might turn out to be better for cell-replacement therapy. "Too much is at stake to pick a favorite cell type yet," she said. "Our favorite is the one that will lead to better treatment."