Period pain has long been ignored. That’s changing.
Researchers are finally trying to understand the complex causes of menstrual pain, or dysmenorrhea—and potential solutions.

When Niara Webb was 15 years old, she experienced period pain so debilitating that she passed out during a church service. When she came to, she was surrounded by people who thought she’d experienced a religious awakening. “The whole time I was just thinking, I just need some Advil,” she remembers.
Now 27, Webb has experienced what she describes as “horrible” menstrual cramps since she first started her period. “I just lived a life of my period cramps are just kind of bad, and that's how it is,” she says. Her experience is common: Dysmenorrhea, or painful periods, affect up to 91 percent of individuals of reproductive age—with 29 percent experiencing “severe” pain.
Webb suffers from secondary dysmenorrhea, when painful periods are a symptom of another health issue, like endometriosis, adenomyosis, and fibroids. For Webb, polycystic ovary syndrome (PCOS) was the root cause of her pain, a diagnosis she only received two years ago. Like many women who suffer from secondary dysmenorrhea, her painful periods have impacted her life. She recalls boarding a flight in such agony that she had “that movie moment of ‘Is there a doctor on the plane?’” shortly before she passed out.
Webb’s experience isn’t unusual. Dysmenorrhea has long been treated as a normal part of the menstrual cycle instead of a pain event that needs to be managed. “A lot of women are either told, or they assume, that it’s normal to have painful periods, even if it’s debilitatingly painful where it affects their normal activity,” explains Karen C. Wang, director of the Division of Minimally Invasive Gynecologic Surgery at Johns Hopkins Hospital.
But for women like Webb, there may be hope on the horizon as both medical and cultural perceptions around period pain are starting to shift, leading to new research on its causes and, potentially, solutions. Some researchers are trying to crack the code on who may be more susceptible to dysmenorrhea while others are trying to untangle the complex web of physiological and social processes at the root of menstrual pain.
The complex problem of period pain
While there was initially some interest in the causes of period pain in the 1970s and ’80s, it “dropped off,” says Laura Payne, assistant professor psychology and Harvard Medical School and director of the Clinical and Translational Pain Research Laboratory at McLean Hospital. She hypothesizes that this was because of the availability of NSAIDs (nonsteroidal anti-inflammatory drugs), like ibuprofen, which became widely recommended for period pain.
But Jada Wiggleton-Little, an assistant professor at Ohio State University whose focus is bioethics, says there may be a different reason period pain is ignored. While it may seem counterintuitive, the fact that period pain is common is part of why it isn’t taken seriously.
“It’s not like someone’s saying, I don’t believe you. If anything, they’re saying, 'Yeah, it’s a period. Of course it hurts,'” says Wiggleton-Little. She has a term for this: pain-related motivational deficit, meaning that people believe you are in pain, but some are not concerned about it in the same way they would be if you were reporting something like chest pain.
“It’s just a fancy philosophical way of saying your pain is believed, but for whatever reason, people are not concerned by the pain that you’re sharing in the way that they ought to be.” In other words, doctors believe that dysmenorrhea is painful, but that pain has been so normalized that they’re not motivated to treat it.
Pain-related motivational deficit may be one of the reasons that period pain has been under-researched for decades, but in the last 10 to 15 years, that’s started to change. Payne says that in 2011, some pivotal research, including a commentary published in the academic journal Pain titled “Don’t dismiss dysmenorrhea!” was a turning point. The authors noted that “dysmenorrhea has been virtually ignored by the pain community,” with few extant studies, despite the large number of women who suffer from debilitating period pain. They described the medical landscape as “appalling,” particularly since dysmenorrhea was, even then, linked to chronic pain later in life.
Since then, there’s been slow but building interest in solving the problem of period pain, particularly severe period pain and the health and social complications it’s linked to.
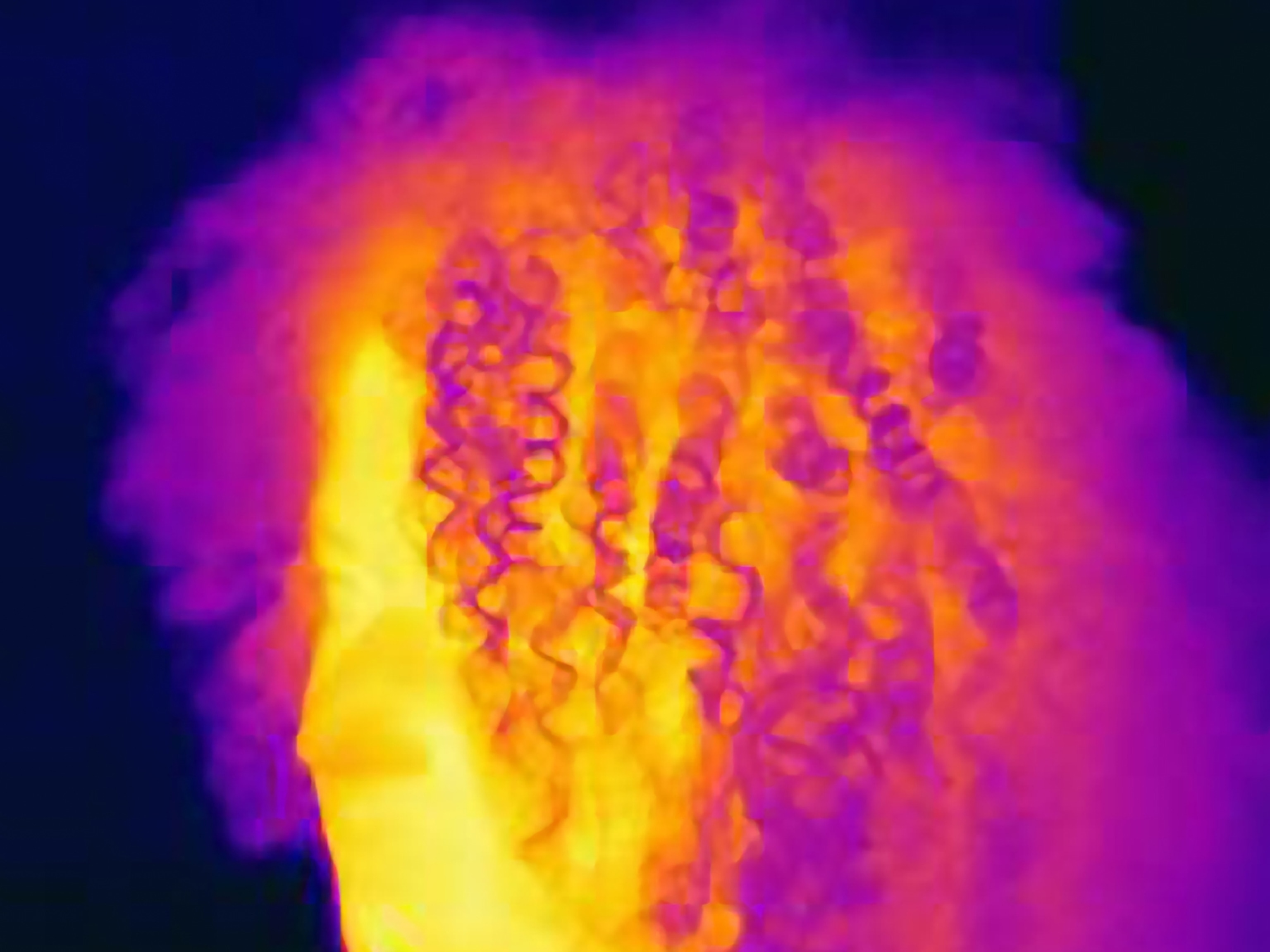
Payne’s research focuses on the role of the brain and the central nervous system in the experience of pain. “What the research has shown is that people who experience moderate to severe menstrual pain also tend to be more sensitive to pain in general,” she says, and this may help researchers identify girls who are more at risk for developing menstrual pain even before their first period.
That was the aim of a research paper published in Pain in 2025. Researchers at the Gynecology Research Lab in Evanston, Illinois, tried to figure out who might be susceptible to pain before they even got their first period, which, for most girls, happens around 11 years old. Of the 207 participants, those who reported “bothersome somatic symptoms” like headache and dizziness were more likely to have widespread pain in the future. More surprising, those who were more sensitive to unpleasant—not painful—stimuli in the lab (like loud noises and flashing lights) had higher odds of developing widespread pain too.
This is important work, especially since period pain can disrupt a girl’s life. Research published in npj Science of Learning found a link between teenage girls with period pain and/or heavy periods and lower exam scores, as well as more time out of school. Menstrual pain was associated with missing 1.2 more days of school a year. A 2025 study from the University of Oxford found that 15-year-old girls who had severe period pain had a 76 percent higher risk of having chronic pain by the time they reached their mid-20s.
Period pain can also impact brain processing for both women and girls. Studies have shown that chronic pain can alter cognitive function, and Payne’s research is revealing that pain can change the way the brain processes information. “When the brain receives a lot of repeated information that something is painful, it shifts into a lot of emotional processing around that,” she says. That can change how information gets shuttled from one area of the brain to another. The result is a heightened experience of pain. “It creates this vicious cycle,” Payne says.
Payne says that the research on dysmenorrhea shows that “pain is a complex experience, with the potential for many different factors that influence that experience, including things that are happening in the body (like hormonal changes) and what is happening in the brain.” She adds that dysmenorrhea is not just uterus-specific but far more complicated; understanding just how complex it is might have implications for broader pain research.
Period pain, Payne says, is a key variable in health studies that may seem unrelated to menstruation, especially since pain sensitivity changes over the course of the menstrual cycle. “This is really impacting how we understand these results in relation to women at different life stages,” she says. For example, if researchers were looking at adolescent girls with or without depression, it would be important to know if any of them had dysmenorrhea.
“We’d want to make sure that we’re accounting for that, because it may be that there are structural changes [in the brain] that are different in adolescent girls who have menstrual pain,” Payne says.
(The menstrual cycle can reshape your brain.)
The future of managing painful periods
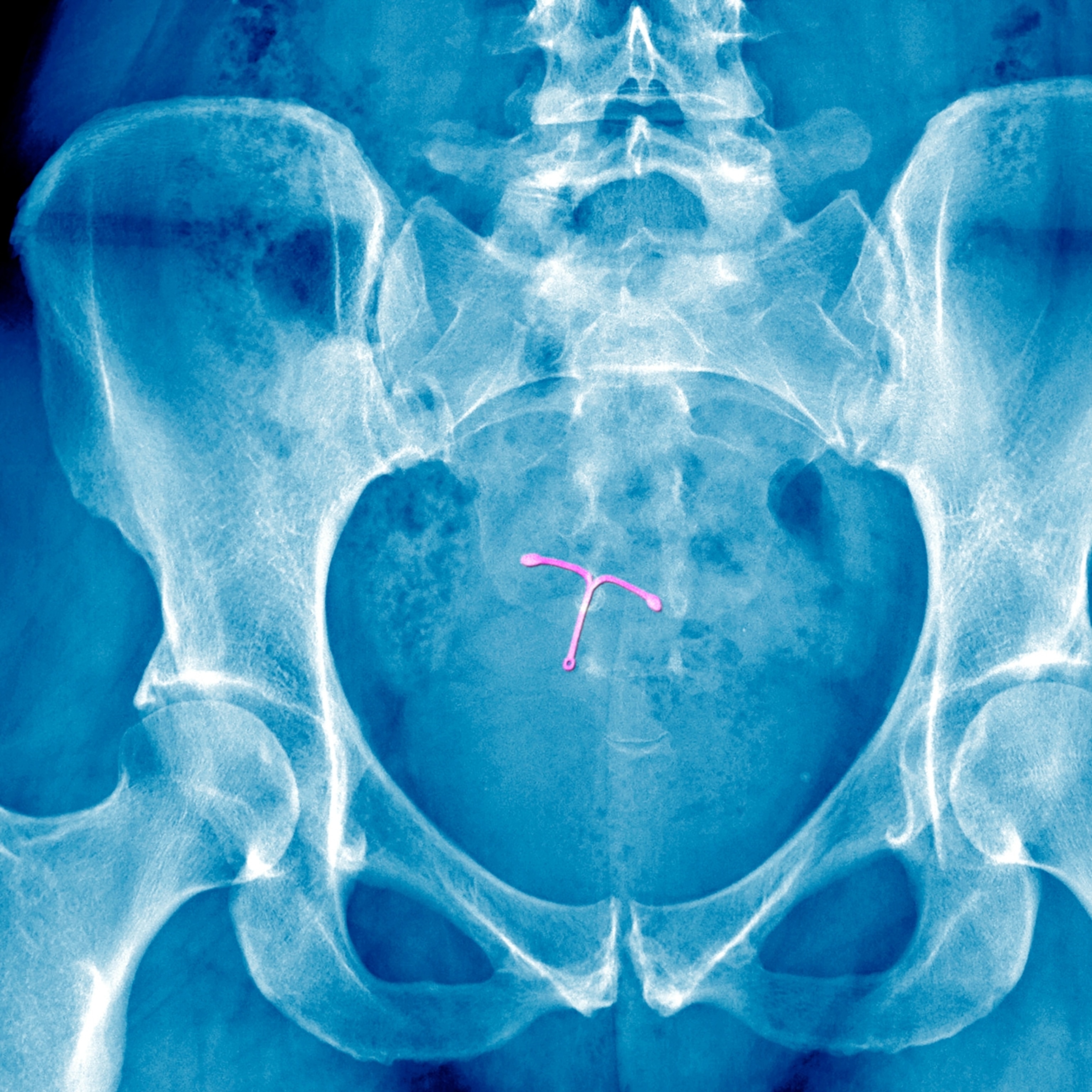
The traditional recommendations for dysmenorrhea currently include managing lifestyle factors like reducing stress and exercising, as well as using heating pads, NSAIDs, and hormone therapies like birth control. In some cases, cognitive behavioral therapy and pelvic floor therapy may be helpful, Payne adds.
Payne is currently in the middle of a study aimed at better understanding why some women don’t respond well to pain relievers for menstrual pain and whether a more sensitive centralized nervous system could be playing a role. This could ultimately lead to better treatments for the 18-20 percent of women in this group, who may experience frustration and overall disruption to their lives, Payne says.
But pain, including menstrual pain, can be tricky to define and treat, largely because it is a mosaic that makes it deeply personal. A review of the field in the journal Pain noted that “individual differences in pain” are the result of “biological and psychosocial variables” that include “demographic variables, genetic factors, and psychosocial processes.”
That observation has held true in recent research on managing period pain. In a 2024 trial of 150 women with premenstrual syndrome (PMS) or premenstrual dysphoric disorder (PMDD) between the ages of 18 and 45, a placebo reduced the intensity of PMS symptoms and interference in their social, educational, and working lives “considerably.” Published in BMJ Evidence-Based Medicine, the study found that those who received the placebo along with an explanation of its intended effects experienced a 79.3 percent reduction in symptom intensity compared to women who had their usual treatment, who reported a 33 percent reduction.
The study found patients responded to “full transparency” without “substantial side effects.” It was a provocative finding, especially considering that women suffering from secondary dysmenorrhea and PMDD are often given poor medical care for these conditions. A recent report from the U.K.’s Women and Equalities Committee found that there was a “pervasive stigma” around reproductive-related pain that left women and girls enduring unnecessary years of agony.
Payne is studying how to quickly establish causes of secondary dysmenorrhea that can often take years to be diagnosed. “For many girls and women, they eventually get there, but they’ve been suffering for too long,” Payne says. “What I think can be a real move in the right direction is shortening the time that a person is able to get the treatment that they need.” Part of the problem, Payne says, is that providers currently take a trial-and-error approach, like prescribing birth control or telling patients to take NSAIDs before finally referring them to a gynecologic specialist that can test for secondary causes.
In the meantime, new treatments for both primary and secondary dysmenorrhea are emerging. Research out of Spain published in the International Journal of Osteopathic Medicine found that an osteopathic manual therapy protocol like rhythmic massage combined with body awareness sessions where participants learned about basic physiology, the menstrual cycle, and dysmenorrhea can improve pain and other symptoms in women with period pain.
Payne, for one, is excited about some of these ideas, including one small but compelling 2020 paper in the journal Pain Medicine. It found that transcranial magnetic stimulation, a type of neurostimulation to increase connectivity in certain brain regions, could provide pain relief for people with primary dysmenorrhea. A more recent, though equally small, 2025 study in the journal Pain came to similar conclusions.
“I am enthusiastic about these novel ideas,” Payne says, adding that it’s important to keep in mind that pain is variable—and solutions are never one-size-fits-all.
Rectifying the cultural disregard for women’s health
Payne considers the lack of research around period pain as a key example of the decades-long “cultural disregard” for women’s health issues. She points to menopause as another example. Wang also sees similarities between dysmenorrhea and menopause in that “women just suck things up,” she says. That attitude reflects Wiggleton-Smith’s pain-related motivational deficit, even though period pain has real material impacts. Studies have shown that period pain is one of the leading causes of missing school and work, associated with the loss of 600 million hours a year. In the United States, that’s roughly a loss of two billion dollars a year.
Until there’s a tangible long-term solution, Webb manages her PCOS symptoms, including cramps, back pain, and migraines, with Nexplanon, a birth control implant, in addition to lifestyle modifications like diet, exercise and regular checkups, and over-the-counter pain medication as needed. For women experiencing period pain, Webb has advice. “There’s no need for anyone for any reason to be going through life feeling discomfort or feeling like they have to hide or feel ashamed of what they’re experiencing,” she says.
Wang agrees: “Most importantly, women shouldn’t have to suffer.”